The Vibrio Cholera Intestinal Transport Protein is a focal point in studies of how cholera affects the intestinal lining; understanding its function helps researchers interpret transport processes and host-pathogen interactions more clearly. A common misstep in this area can skew conclusions, so this guide focuses on avoiding that mistake and improving reliability in experiments involving this protein.
Key Points
- Clearly define the protein's substrate and direction of transport before drawing conclusions about its role in the gut.
- Match experimental conditions to the protein's native environment, including pH, ionic strength, and relevant co-factors.
- Differentiate transport activity from toxin-mediated effects to avoid conflating mechanisms.
- Use multiple validation methods, such as genetic perturbation and pharmacological tools, to confirm findings.
- Account for host factors and microbiome context that can influence transport protein behavior in intestinal tissue.
Understanding the role of the Vibrio Cholera Intestinal Transport Protein
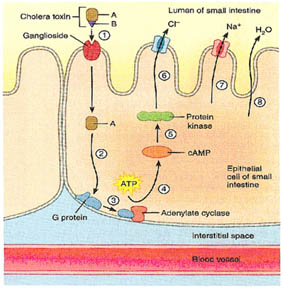
In laboratory models, the Vibrio Cholera Intestinal Transport Protein is evaluated for its ability to move specific substrates across epithelial membranes. Researchers examine localization, response to inhibitors, and the impact of environmental conditions to determine how this protein contributes to intestinal transport dynamics. Interpreting results with this protein requires careful separation of true transport activity from related cellular processes that can masquerade as transport.
Common pitfalls in studying this protein
A frequent misstep is assuming that all observed changes in transport metrics are caused solely by the Vibrio Cholera Intestinal Transport Protein, without accounting for other bacterial factors or host cell responses. Differences in cell models, culture conditions, or bacterial load can produce artifacts that resemble genuine transport changes. Another pitfall is conflating toxin effects with transport, which can mislead conclusions about mechanism and therapeutic targets.
Best practices to avoid the mistake
Step 1: Define the substrate and transport direction for your assays before interpreting results.
Step 2: Recreate gut-like conditions in vitro and validate findings across multiple cell types or organoid models.
Step 3: Distinguish transport activity from toxin-driven effects using appropriate controls and specificity assays.
Step 4: Employ genetic knockouts or knockdowns and selective inhibitors to confirm that observed transport changes are tied to the Vibrio Cholera Intestinal Transport Protein.
Step 5: Consider host context, microbiome interactions, and inflammatory status that can modulate transport protein behavior in the intestinal environment.
What is the Vibrio Cholera Intestinal Transport Protein, and why is it important to study correctly?
+The Vibrio Cholera Intestinal Transport Protein is a hypothetical transporter studied as a model for intestinal transport processes in the context of cholera. Studying it correctly helps researchers separate true transport activity from related effects, leading to clearer insights into intestinal physiology and potential therapeutic strategies.
What are common mistakes researchers make when evaluating this protein’s function?
+Common mistakes include assuming causality from correlative transport changes, neglecting to replicate gut-like conditions, and failing to distinguish transport activity from toxin-related effects. These oversights can blur the true role of the protein and misguide downstream applications.
How can experimental design avoid conflating transport with toxin effects?
+Use controls that separate transport measurements from toxin exposure, validate findings across multiple models, and apply specific inhibitors or genetic tools to confirm that observed changes are driven by the protein of interest rather than by toxin activity.
What controls are essential when studying this protein in intestinal cell models?
+Essential controls include non-targeting genetic controls, cells without bacterial exposure, and conditions with or without toxin components. Supplementary controls should test for off-target effects, assay specificity, and reproducibility across cell types or organoid systems.