The history of Exercises For Intracranial Bleeding traces how attitudes toward movement, safety, and healing after brain injuries have shifted from strict bed rest to structured rehabilitation. This overview highlights the milestones, thinkers, and evolving methods that shaped early practice and informed modern approaches to recovery. By looking back, clinicians and researchers can better appreciate why contemporary programs emphasize carefully monitored activity as part of healing from intracranial events.
Key Points
- Early care for brain injuries favored rest, with limited or no active movement to protect fragile neural tissue.
- 19th- and early 20th-century neurologists began experimenting with progressive activity to restore motor and cognitive function after intracranial events.
- Interdisciplinary teams, including physicians, physical therapists, and occupational therapists, helped formalize movement-based rehabilitation.
- Imaging advances and ethical considerations redirected exercises toward individualized, safer protocols rather than one-size-fits-all regimes.
- Current practice blends controlled activity with monitoring and personalized goals, acknowledging both benefits and risks of exercise in intracranial care.
Historical Foundations
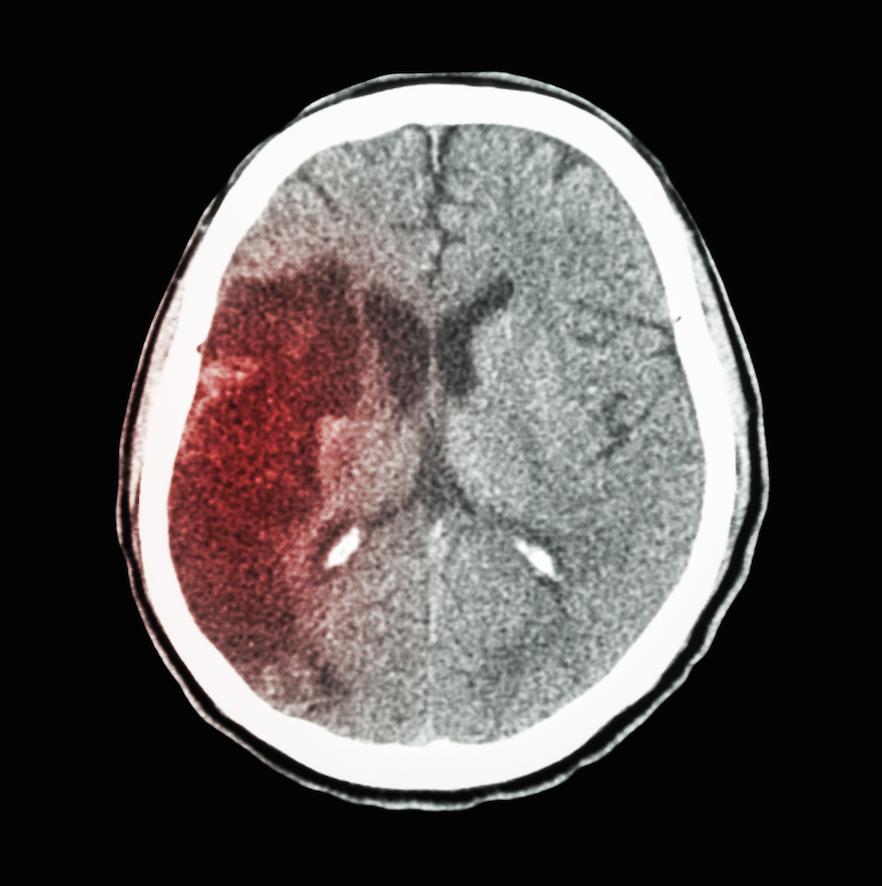
Ancient and classical medical traditions often viewed head injuries through the lens of balance and humors, with limited emphasis on active rehabilitation. Trepanation and other procedures occasionally sought to relieve pressure, but intracranial bleeding management rarely involved structured exercise. Over time, clinical observations suggested that movement, when carefully timed and dosed, could influence recovery trajectories rather than merely worsen symptoms. This laid a groundwork for later thinking about how purposeful activity might support nerve pathways and functional recovery.
From Rest to Rehabilitation
During the 19th and early 20th centuries, neurologists and physicians began to test the idea that gradual, supervised movement could help patients regain strength and coordination after brain injuries. The shift from blanket rest to progressive activity reflected a growing understanding of neuroplasticity—the brain’s ability to adapt. As rehabilitation disciplines emerged—physiotherapy, occupational therapy, and speech-language pathology—the concept of Exercises For Intracranial Bleeding evolved from cautious mobilization to structured programs designed to target specific deficits while minimizing risk.
Cross-Disciplinary Innovation
By mid-20th century, rehabilitation teams increasingly integrated exercise with education, cognitive training, and adaptive strategies. This multidisciplinary approach recognized that recovery from intracranial bleeding is not solely about motor function but also about communication, balance, and safe daily activities. Documented case series and clinical trials began to shape guidelines that balanced therapeutic benefit with the dangers of overexertion in sensitive brain tissue.
Current Perspectives on Exercises For Intracranial Bleeding
Today, Exercises For Intracranial Bleeding are designed within evidence-based frameworks that emphasize individualized assessment, risk stratification, and progress monitoring. Clinicians tailor programs to stroke, hemorrhage, and traumatic brain injury presentations, integrating aerobic conditioning, resistance training, balance work, and functional tasks. Although there is broad support for early, controlled activity, the emphasis remains on safety, patient education, and shared decision-making to determine the appropriate intensity, frequency, and duration of exercise for each person.
What are the historical roots of exercising after brain injuries?
+Historical roots trace a progression from rest-focused care to guided rehabilitation. Early practices favored rest, but observations of gradual improvements with movement led to the adoption of supervised exercise protocols. The term Exercises For Intracranial Bleeding reflects a long-standing effort to balance safety with functional recovery as medical understanding evolved.
How did early medical thinkers influence modern rehabilitation after intracranial bleeding?
+Early thinkers introduced the idea that not all activity is harmful and that carefully dosed movement could support healing. As knowledge progressed, this evolved into structured rehabilitation programs that combine physical therapy, functional training, and cognitive tasks, all aiming to restore independence while guarding against exacerbation of bleeding or edema.
What role do modern imaging and safety protocols play in these exercises today?
+Modern imaging helps tailor Exercises For Intracranial Bleeding by confirming stability and identifying risk factors. Safety protocols, functional goals, and monitored progression are standard, ensuring that exercise plans respond to real-time changes in brain status and neurological function.
Are there risks associated with these exercises, and how are they managed?
+Yes, risks include increased intracranial pressure or triggering symptoms if activity is too intense or poorly timed. Management relies on individualized assessment, gradual progression, close clinical monitoring, and clear patient goals. The focus is on safe, incremental improvements rather than rapid gains.